Dentists solving your healthcare needs?
You’re experiencing painful sensations in your mouth and your GP has told you ‘It’s just an ulcer, use some Bonjela and it’ll be fine!’ You used it and feels no better. ‘My GP said it’s fine… a dentist will know no better, right?’ Wrong!
While GPs are experienced and knowledgeable medical practitioners, a dentist specializes in your head an neck. In other words, they specialize in areas of the body that one always goes to a GP about.
Samantha was a 13 year old girl from Sussex. She has been experiencing diarrhoea, mild abdominal pain nausea and weight loss; she has just come back from a holiday in Mexico. When seeking advice from her GP, she was told that she likely had food poisoning and should allow for symptoms to fade. However, during a routine checkup at her orthodontist appointment, her dentist noticed something abnormal. She had inflamed ulcers in her mouth and the dentist had a hunch of what condition she may have…Crohn’s disease. After a few tests that the dentist referred her to get, Samantha got a diagnosis of Inflammatory Bowel Disease, just as her dentist thought.
Whilst it is true that 80% of the time GPs can successfully diagnose their patients, the public is unaware of how diseases can commonly present themselves predominantly in the mouth of which dentists have expert knowledge in.
It is for this reason that the NHS must provide more funding to dental practitioners, not only so that they can better treat more people but do so with the best equipment and therefore obtain a better outcome.
I was able to interview Dr Babber, an experienced dentist who does both NHS and private work and owns several practices. ‘I was saddened that I was forced to give young adults dentures instead of good quality implants that the NHS couldn’t provide. This is why I chose to do private work as well so that I could feel that I was able to treat patients with full potential and know that I was giving them the best treatment possible’. It is evident from his statement that not enough awareness is focused on the dental community as most people look to GPs and hospital workers for medical advice only. But why is this?
I took it upon myself to discuss with family and friends about why they feel that dentists are not as medically qualified as they truly are. Most people conveyed that they don’t know of any dentists who are able to share that information with them. Others said that there are simply many more GPs and hospital workers than dentists, therefore people will prefer to go to them with head and neck concerns. This prompted me to look up if there truly is a shortage of dentists in the UK and to no surprise… there is. In fact, experts are warning of a growing shortage of dentists, with the number of new recruits falling by a fifth in just two years. The Telegraph reported that ‘there are a rising number of dental practices only taking private patients, along side a sharp drop in those offering purely NHS care.’ This coincides with Dr Babber’s concern for lack of NHS funding and reinforces the fact that more medical students should consider dentistry as this increase may prompt the NHS to invest more money into dentistry.
The course for dentistry does not differ hugely from general medicine training. As it happens, the first three years in the five year dental course is medicine only and the following two years focus on head and neck. A dental student should indeed have medical work experience for example: care homes, pathology labs, etc as well as perhaps two weeks in a dental practice. A degree in Dentistry is required but any other medical or scientific qualifications could serve useful in this profession. Just like medicine, high grades are needed. The minimum grades for A levels include ABB and chemistry is required, just like medicine.
When speaking to Dr Babber about what factors drove him to dentistry not medicine, he answered ‘I had family members with medical issues and doctors couldn’t always help. I always wanted to be able to help a person in some kind of way. I was always very artistic and knowing that I could fix a smile or boost a person’s confidence with my hands gave me great joy. I also enjoy using Digital Dentistry to map out what a set of teeth can look like and I enjoy the journey to achieve that and so do my patients. I knew that I would always be able to leave patients in a better state than when they came to me…when doctors can’t always. ‘
Effects of COVID—19 on the Dental Community
Is there decay that you don’t know about or do you need a brace to fix your congested mouth? The chances are that you may not be able to get these seemingly normal treatments for many months or perhaps years to come. Standard appointments that didn’t seem necessary in the past may become impossible to get and it may be many years until you find yourself sitting in a dentist’s chair.
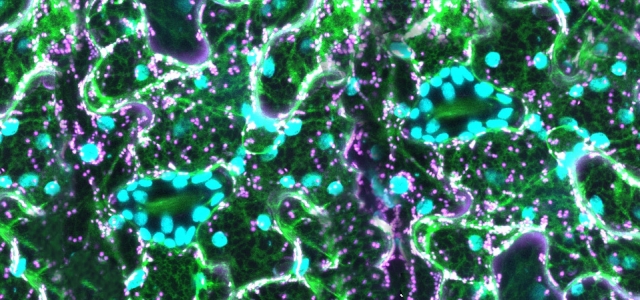
80% of dental work requires a form of aerosol. Aerosols are a suspension of tiny particles or droplets in the air. Aerosol transmission has been defined as person to person transmission of pathogens through the air by means of infectious particles. With 80% of treatments unable to continue, dentists had to make use of video conferencing. This created a huge back log of patients as surgeries were working at 20% capacity. When the government announced that dental practices could reopen on the 8th June, many dentists were extremely wary due to the fact that there was a shortage of funding which was needed for equipment and staff.
In addition, there was an uncertainty of threat level as aerosol procedures— whilst reduced—still bring high exposure to dentists and patients. Whilst the NHS still paid dentists through the period of working from home, they only did so with the knowledge that the employee would video conference and be available for reemployment. However, private practices did not have this security and so it is thought, that due to the lack of income from patients, many will be forced to close and business will be lost for many private practice owners. Although some practices are open, there are many safety precautions that have been put in place to minimize the transmission of COVID19. For example: only patients in pain or in a severe state will undergo treatment using aerosols and patients must fill in a questionnaire about their current health. The real killer in the guidelines is a fallow time of 60 minutes for floor cleaning at the end of each session between patients and reopening windows. This has reduced patients seen per day from 30 to 5.
Will this pandemic destroy dental businesses?
There is still not enough information about the virus and predictions can in no way give an accurate idea of how dentists should prepare; this is pandemic is like no other. Dr Babber, a dentist and private practice owner who I interviewed expressed that whilst a vaccine is still not in use, there can be no certainty in how transmission rates and death rates will be altered and even when it is in use, there are still doubts about how long and effective immunity will be. He said that he thinks that it is likely that there may be a second spike in death rates in the coming months so many dental practice owners , including himself, are investing in extractors and blowers with no delay. They force air outside and bring negative pressure in the room which will reduce the transmission of the virus even when aerosols are in use. Whilst spending huge amounts of money and protective PPE is not ideal in this time of desperation and shortage of money, it is necessary to give the dental community a chance of carrying on.