Dive into the fascinating world of embryonic stem cells, where groundbreaking medical possibilities meet complex ethical debates, and discover how this cutting-edge research could revolutionize the future of healthcare.
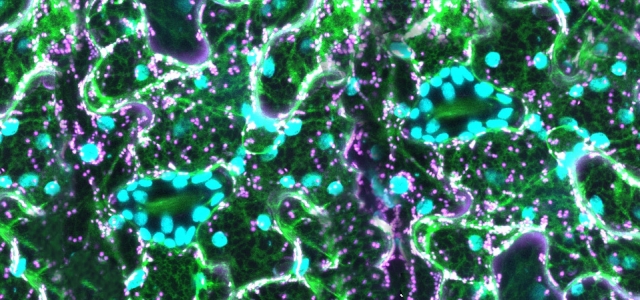
The dictionary defines an embryonic stem (ES) cell as a cell capable of differentiating into any type of body cell. Embryonic stem cells are derived from the early stages of an embryo at just a few days old. In humans, mice and other mammals, at this stage the embryo is a ball of approximately 100 cells. It is known as a blastocyst and has two parts: the trophectoderm and the inner cell mass.
Each part has a completely different function. The Trophectoderm forms the placenta that supports the embryo as it grows inside the uterus while the inner cell mass is a ball of 10-20 undifferentiated and unspecialised cells. These cells will multiply and differentiate extensively to make the various cell types needed to form the entire animal. Some of the cells in the inner cell mass are pluripotent, meaning they can become any type of cell in the body.
ES cells in mice: A study of what they can do
Mouse ES cells can be put back into a mouse blastocyst and this blastocyst can then be returned to the uterus of a female mouse to develop into a foetus. The injected ES cells take part in the development of the foetus and the resulting pup is born with a mixture of cells from the host blastocyst and cells that came from the injected ES cells. This produces mice with modified genes. This new mouse with cells from two different origins is known as a chimera.
Chimeras can pass on modified genes to their offspring and scientists can use these mice to study genes of diseases. For example, scientists produced mice with mutations found in human cancers enabling them to study how cancers grow and to test drugs. A Nobel Prize in Medicine was awarded to the three scientists who pioneered genetically modified mice.
What’s the fuss about?
The use of these cells would overcome the problems of donor tissue shortage and implant rejection, if the cells are made immuno-compatible with the recipient. They could be used to replace cells that have been damaged or destroyed, as seen in:
- heart disease where ES cells become new muscle cells and beating heart cells
- type 1 diabetes where ES cells can be used to produce insulin
- cases of spinal cord or brain injury, including multiple sclerosis, that have led to paralysis where ES cells form human nerve cells and myelin
- cases of cure Parkinson’s disease, strokes, Alzheimer’s disease and many more diseases, where specialised ES cells become the missing necessary cells
There are approx 100-150 million people in the United States alone who would benefit from the use of stem cell-derived treatments which could find a solution to their health problems.
The ethical concerns
Embryonic stem cells pose a moral dilemma. Do we prioritise the duty to alleviate or prevent human suffering, or do we prioritise the duty to respect the value of human life? There is no way of doing both; to obtain embryonic stem cells, the early embryo has to be destroyed. This means destroying a potential human life. But embryonic stem cell research could lead to the discovery of new medical treatments that would alleviate the suffering of many people. This moral dilemma is one of the main reasons why no clear-cut decisions have been made about embryonic stem cells and its research. Researchers believe that a foetus doesn’t develop the concept of pain until around the 20th week of gestation, but the potential to become a human being means that many disagree with the embryo being destroyed. Many religions believe in the sanctity of life which means that embryonic research would be disrespectful and against their beliefs. However, many embryos are frozen or discarded after IVF so there is little chance of them becoming alive or being put inside a uterus. In these cases, many believe that the embryos will be better used to try to cure diseases and improve quality of life.
The cons of using ES cells
As well as the concern about the ethics, many people are also worried about the lack of understanding of the possible side effects. As these treatments have not been around for long, it is impossible to know whether there will be related health problems in the long run. There is also the issue of rejection, however, because ES cells contain less immune-related surface proteins, this is a problem that can be overcome.
Another problem is the treatment obstacles and lack of testing present, ironically because people are worried about the other concerns. Reports of successful clinical treatments using embryonic stem cells are limited. Challenges include unstable gene expressions, tumour formation, and difficulty activating cells for specific purposes. Scientists believe that these problems can be solved though, given time. On the other hand, some people believe that it doesn’t make sense to continue harvesting embryos when the failure rate remains so high. Many believe there is a future for embryonic stem cells, just not yet.
The legislation
The US government strictly prohibits any activity of stem cell research or human cloning. Private companies, which already have the possession of many cell lines, wouldn’t hesitate to defy all the norms and ethics pertaining to this research however. Currently, the Food and Drug Administration (FDA)’s approved ES cell uses are for leukaemia, lymphoma, neuroblastoma and multiple myeloma-fields where it is agreed that the positives outweigh the negatives. The UK allows embryo research up to 14 days for specific purposes, including increasing knowledge about embryo creation and development. The HFE Act of January 2001 permits research for therapeutic purposes using cells derived from human embryos.
In conclusion, embryonic stem cells are an exciting new field that holds boundless possibilities for curing diseases. For example, children that have an immunodeficiency disorder and receive this form of treatment see a success rate of 90% today, and that figure continues to grow. In cases like this, the positives outweigh the negatives. However, there are many ethical concerns as well as varying success rates that mean that they are not yet reliable. An exciting new future is on the horizon, but there are more discoveries to be made before we reach it.
Sources:
Juliet explored a number of websites to research the topic of this blog including:
- Biology Wise
- BBC bitesize
- ScienceDirect
- Verywellhealth
- Oxford academic
Some of her knowledge was obtained at school and from the the Wellcome Sanger Institute. Juliet’s school has been supported to participate in the Youth STEMM Award thanks to sponsorship from Wellcome Connecting Science.